FAILURE TO REPLACE
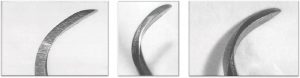
Problem: Improper Sharpening
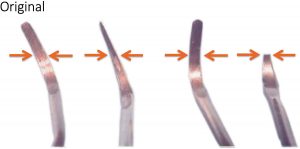
Problem: Beyond Life Expectancy
What criteria do you utilize when deciding to replace a scaler? The condition of the working end? Broken blades? Your curettes have become sickles from an incorrect sharpening technique or the knowledge of the physical and often irreversible effects on your body when using a scaler that is past its ‘use by’ date? What about the consequences of using a compromised scaler on a patient? Do these facts affect your decision on when to replace?
As an Educator, one of the most frequently asked questions I receive is….’How long does a scaler last before it should be replaced?’ The answer to this question unfortunately lies within the abyss of answers to questions such as “How long is a piece of string?” or “Where did my other sock go that was in the dryer?”. The current recommendation is that when 20% of the instrument blade width or length is reduced or no longer the original design, it is time to replace the instrument. How long it takes for each instrument to reach this threshold is dependent on factors such as:
- The frequency of use: how many setups of instruments are available and how many times per day each is used, as well as how many days per week are
- Difficulty of patients (quantity and tenacity of the calculus)
- Use of ultrasonic devices
- Frequency of sharpening as well as proficiency of sharpening
- Use of instruments only for the intended use
- What material the blades are made from (Immunity Steel Vs Emerging Technology)
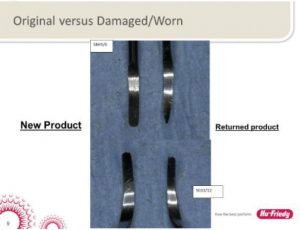
Breaking It Down: Cost per Use
Unfortunately, more often than not, scalers are often looked at as a lifelong part of the furniture when they should be classified as a consumable commodity in practice assets and order budgeting. Every time a scaler is used, the blade dulls and requires maintenance sharpening. Over time, the working end of the scaler will reduce in length and width. Continued usage of a scaler with a reduction greater than 20% in the working end increases the risk of instrument breakage subgingivally as well as decrease adaptability of the blade to the surfaces the instrument is intended for leading to tissue trauma and operator fatigue. Instruments are ergonomically designed to be used in optimal conditions for both patient and clinician’s comfort and safety.
Scalers that are sharpened infrequently may have a “longer” lifespan resulting in less frequent replacement and associated costs however, what are the associated cost and risks of a dull, sub-optimal scaler? Let’s look at what we already know: An instrument in sub-optimal condition is ineffective and inefficient. The scaler will have reduced tactile sensitivity which can lead to the inability to detect or remove deposits and an increase the likelihood of burnished calculus and slipping while trying to remove it. Increased lateral pressure and number of strokes are required to remove the deposits which affects both the patient’s comfort as well as fatiguing the clinician’s hand, wrist, arm and shoulder. The increased number of strokes required can take more time during the appointment than it would to sharpen the instrument prior to use.
In a hypothetical scenario, let’s say a clinician is working 5 full days per week. The scalers are used and processed 3 times per day. At the 12-month instrument check – let’s also factor in 4 weeks holidays per year where the instruments are not being used, the working end has lost 20% of its’ length and/or width. At a price of $80 per instrument, the scaler will cost approximately .13 cents per use.
What other consumable commodities do you use in your daily practice that would have an equal value? For example, the average cost of a prophy cup is .65. That’s worth 5 instruments!
The Costs for the Clinician
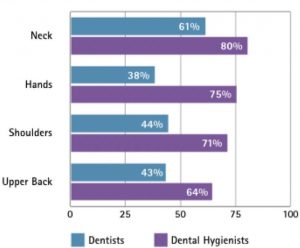
A literature review2 conducted by Johnson and Kanji in 2016 states that 92% of Dental Professionals reported symptoms in at least 1 anatomical, upper body region in the past 12 months with Dental Hygienists being the group most affected (see Fig 1). Work related Musculo-skeletal Disorders (MSD) in dental hygienists are often blamed on repetitive movements, awkward and static postures, pinch- grasp, forceful exertions, vibration, poor ergonomics, and insufficient breaks amongst other factors.
So how does a dull or compromised instrument contribute to a MSD?
Dental Hygienists often perform over 30 repetitive strokes per minute, increasing their risk for muscle strain 3.4 Factor in using a small diameter, a heavier weighted handle and/or a dull or sub-optimal blade results in increased pinch-force and lateral pressure required to remove deposits 3,5,6,7. Over time, the repetitive strain and cumulative trauma subsequently cause clinicians to seek out both traditional and complementary treatment modalities to manage pain, reduce their workload or in extreme cases, leave the profession due to MSD’s 8,9
And The Patient
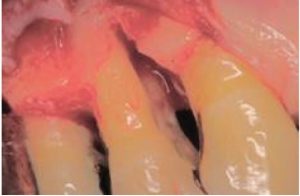
As previously mentioned, a dull or compromised scaler can lead to increased discomfort and decreased tactile sensitivity due to increased lateral pressure and number of strokes needed to remove the deposits. The cost of burnishing calculus, resulting in iatrogenic and supervised progression of periodontal disease when patients are placing their oral health in our hands cannot be measured (Fig 3,4). Breakage of a blade in a patient’s mouth, with possible need for surgical intervention due to using an over-worn working end is a preventable situation with a simple and quick check of the working end against a template.
What can we do?
When having discussions with workshop participants, I have discovered that a large number of practitioners do not routinely sharpen their instruments on a daily basis with the most common reason being that they simply do not have the time. If sharpening is performed routinely, the process should only take a minute or two per kit at each appointment – less time than trying to removed calculus with
a dull blade. When performing subgingival debridement, a sharpening stone sterilised with the instrument setup will make it easier to debride as you go. Scalers should be sharpened before every patient for efficient and effective appointments3. To quote Periodontist Dr Victor M Sternberg, ‘Curettes should be replaced regularly and instrument sharpening is not optional to be a successful (clinician)’. Would you use a dull bur to prepare a tooth for a restoration?
Choosing appropriate instruments with considerations for the weight and handle design, wider than 11m with either a criss-cross or knurled surface reduces the need for pinch-grip and over exertion 7.
A routine, quick assessment of your scalers against a template (Fig 2) is a simple way to ensure neither you nor your patients’ health are being compromised and that you can continue to provide care in a safe and healthy environment. This check can be completed by the clinician or nurse prior to instrument processing. Scalers need to be valued as consumable stock to ensure clinicians feel confident and empowered to maintain them without the pressure to try to make them last longer.
Worried about how to dispose of your worn instruments? Hu-Friedy Australia / New Zealand have a recycling initiative conducted when attending relevant dental conferences with details emailed to dental practices prior to the events.

Bibliography
- Rucker LM, Sunell S. Musculoskeletal health status in BC dentists and dental hygienists: Evaluating the preventive impact of surgical ergonomics training and surgical Vancouver: Workers’ Compensation Board of British Columbia; 2000. pp. 1–91.
- (PDF) The impact of occupation-related.. Available from:
https://www.researchgate.net/publication/317224618_The_ impact_of_occupation-related_musculoskeletal_disorders_on_ dental_hygienists[accessed Jul 19 2018].
- Sanders MA, Michalak-Turcotte Strategies to reduce work- related musculoskeletal disorders in dental hygienists: two case Work-related MSDs and dental hygienists 79
Can J Dent Hyg2016;50(2):72-79 studies. J Hand Ther. 2002;15(4):363–7
- Branson BG, Black MA, Simmer-Beck M. Changes in posture: A case study of a dental hygienist’s use of magnification loupes. Work. 2010;35(4):467–76
- Michalak-Turcotte Controlling dental hygiene work-related musculoskeletal disorders: the ergonomic process. J Dent Hyg. 2000;74:41–48
- Kerschbaum WE, Liskiewicz Cumulative trauma disorders: an ergonomic approach for prevention. J Dent Hyg. 1997;71(4):162–67
- Rempel D, Lee DL, Dawson K, Loomer The effects of periodontal curette handle weight and diameter on arm pain A four-month randomized controlled trial. J Am Dent Assoc. 2012 Oct;143(19):1105–13
- Akesson I, Johnsson B, Rylander L, Moritz U, Skerfving S. Musculoskeletal disorders among female dental personnel — clinical examination and a 5-year follow-up study of Int Arch Occup Environ Health. 1999;72:395–403
- Crawford L, Gutierrez G, Harber Work environment and occupational health of dental hygienists: A qualitative assessment. J Occup Environ Med.2005;47(6):623–32


 Deb is a Dental Hygienist with a Grad Dip in Restorative Dental Hygiene (Canada).
Deb is a Dental Hygienist with a Grad Dip in Restorative Dental Hygiene (Canada).