The Cortical Window
The Computer-Guided Cortical Window Approach
A cortical window (bone lid) access to the apical region is less invasive, minimises bone loss and is less traumatic in comparison to alternative techniques.
The perimeter of the window is determined from radiographs of the area. Radiographs are essential to all aspects of endodontics; however, flat films ore two-dimensional images of three-dimensional structures and so data interpretation is subjective.
Cone beam computed technology (CBCT) enables the clinician to visualise structures in sagittal, axial and coronal planes. Three-dimensional imaging provides more substantial data for diagnosis, pre-treatment planning, post-treatment assessment and reassessment evaluations (Ahlowalia et a l, 20 l 3; Venskutonis et al, 2014).
A printed stereolithographic surgical template can guide the osteotomies during the surgery; minimising deviation from the digital surgical plan. Surgical templates printed from three-dimensional imaging optimise site preparation, the perimeter of the osteotomy, depth of cortical bone, extent of pathology and volume of bone graft required (Kuhl et al, 2015; D’haese et al, 2012; Pinsky et al, 2007; Strbac et al, 2017).

mucosa).



Piezotome Osteotomy
Traditional osteotomies use large, round burs which remove significant cortical bone. Delayed healing, increased post operative pain and other complications may ensue.
With microscopes, piezotomes and ultrasonic tips, a smaller osteotomy is created, thus minimising the aforementioned sequelae.
Piezo surgery enables micrometric saw cuts which preserve cortical bone loss and facilitates preservation of root length by lower resection ang les and enhanced visibility.
In deep spaces, ultrasonic vibrations break down irrigants into small particles readily washed from the crypt.
Less vascular presence in the crypt minimises use of hemostatic agents (Viscostat) and interference with retro-seal setting time . The use of a piezo surgical devices ( Figure 1) enables accurate shaping of the cortical window and diminished osseous removal, in contrast to traditional crypt creations which are freehand guided (Abella et al, 2014).
Case Report
The patient presented to our surgery with a history of ‘sporadic discomfort in the gum’ overlying tooth LR 2.
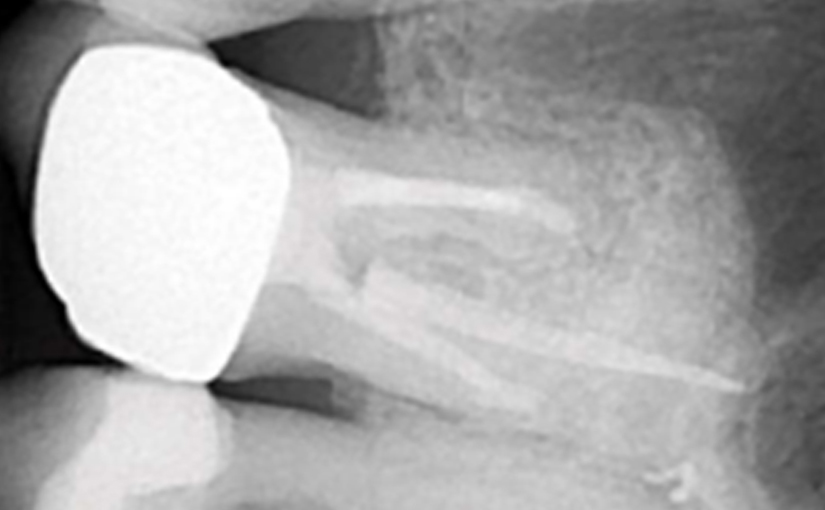
A two-dimensional intraoral radiograph revealed a prior history of root canal therapy and a porcelain-fused-to-metal (PFM) crown (both completed approximately 10years ago) (Figure 2).
Swelling began the evening prior to the appointment; the patient reported that the throbbing necessitated analgesics for relief of the pain. No sensitivity to pressure nor reaction to temperature were noted; the patient could not localise the tooth causing the distress. Treatment options were discussed with the patient; retreatment through the PFM crown was chosen.
Anaesthesia was administered (posterior superior alveolar nerve block – 2% xylocaine with epinephrine 1: 100,00 and infiltration facially and palatally 2% xylocaine with epinephrine l : 50 ,000 ). A conservative access preparation was made; decay was identified proximal to the palatal canal and no fractures or cracks were noted.
Cavil was present beneath the composite core and the untreated MB2 canal ( Stropko, 1999) was discovered.
A reservoir was made in the gutta percho (Proultra ultrasonic tip). Endosolv E was used to soften the gutta percha (Hwang et al, 2015).
After debridement and shaping, Ca(OH)2 (Ultrocal XS) was placed in the root canal space to further enhance disinfection. Prior to obturation, drainage was noted coming from the MB2 canal; drainage was arrested and the canals root was filled with vertical condensation of warm gutta percha (VCWG) and AH-Plus sealer (Figure 3)
The patient returned in six months for reassessment. Tooth LR 2 was within normal limits to percussion, bite, palpation, mobility and probing.
Eighteen months later, the patient returned for a second reassessment appointment (Figure 4 ). Tooth LR2 was slightly sensitive to percussion and the overlying gingival tissues were inflamed.
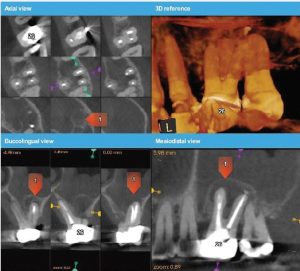
The patient was referred for a CBCT; the scan (Figure 5)







revealed a common area of rarefying osteitis surrounding the mesial buccal and distal buccal roots which had caused elevation of the sinus floor. As the endodontic pathology had not resolved, treatment options were proposed. The patient chose to have microsurgical therapy performed.
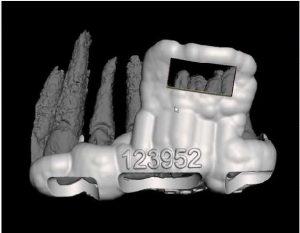
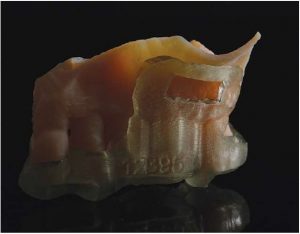
A JD–printed stereolithographic template was created by combining the CBCT scan data with an intraoral scan’s (3Shape Trios intraoral scanner) digital data. The data was then imported into Codiagnostix software in order to plan our approach and design our cortical window dimensions for optima l access to the roots (Figure 6).
The guided microsurgical approach would facilitate an osteotomy design to minimise the potential for sinus membrane perforation. The JD-printed guide for the cortical window would guide the length and angle of the osteotomies using the piezosurgical saw (Figure 7).
Cervical recession and decoy were in evidence about teeth LU and LRI in addition to exposure of the crown margin of tooth LR2.
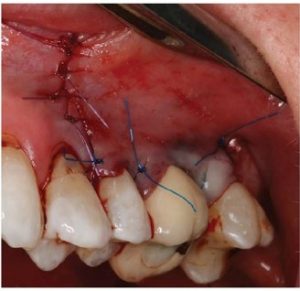
The cervical area of tooth LR3 was severely abraded. An intra -sulcular full-thickness muco-periosteal fap was raised; a vertical re leasing incision was positioned mesial to tooth LRI. The surgical stent was placed over the maxillary teeth (Figure 8) and a piezotome-guided surgical window wasdeveloped using the margins of the stent (Figure 9).
A chisel was used to elevate the cortical plate and root resection performed with Lindemann burs (Figure l0).
The cortical window was placed in sterile saline while the endodontic microsurgery was completed. After resection
using Lindemann burs, the root periphery was stained with methylene blue and examined for anomalies and the root canal space was retro-prepared with ultrasonic tips to a depth of three millimetres, creating a reservoir for the retro sealing materials.
The retro-preparation was rinsed with ethylenediaminetetraacetic acid (EDTA) and dried with paper points.
Bosworth Super-EBA was placed (Figure 11) and the root end burnished with a multi-fluted carbide bur. Radiographs were taken at the retro-preparation stage and the retro sealing stage to ensure accuracy of direction and material placement. The defect thoroughly debrided and was grafted with allograft (Straumonn Allograft) (Figure l 2). The cortical bone window was replaced and ensured to have no mobility (Figure 13)
The flap was closed with Ethicon 5-0 Prolene monofilament sutures (Figure 14) and a post-operative radiograph was taken (Figure 15).
The patient was directed to use 800 mg of ibuprofen and l000 mg of acetaminophen for pain and to rinse with chlorhexidine.
Sutures were removed in seven days and the patient reappointed for reassessment. The re-evaluation radiograph taken at nine months showed substantial osseous regeneration (Figure 16) and a post-operative CBCT scan was taken after one year, showing complete bone regeneration and continuity of the buccal plate. (Figure 17).
Conclusions
Along with surgical operating microscopes and piezotomes integration of optical scanners and CBCT Dicom files to JD–printed stereolithographic surgical guides is yet another iteration in the advancement of endodontic microsurgery
This novel, digitally–guided approach used in this case report, along with the intraoperative use of a JD–printed osteotomy guide, allows for greater efficiency and accuracy for creation of the access window to the roots.
The technique gives the advantage of bone preservation by allowing the cortical plate to be replaced, yet still provides adequate access for the apical root preparation.
The JD-printed guide provides a control for the osteotomies without risking damage to vita l structures. This digitally guided microsurgical approach provides accuracy, access, control and bone preservation to the endodontic apical surgery procedure.
As we come upon the dawn of a new age of digital dentistry, we can see the future applications to be endless.

References
Weller RN, Niemczyk SP, Kim S ( 1 995) Incidence and position of the canal isthmus. Port l . Mesiobuccal root of the maxillary first molar) Endod 21 (7):380-383
Garcia-Guerrero C, Guauque SQ, Molano N, Pineda GA, Nino Borrero JL, Morin-Zuluaga DJ (2017) Predictors of clinical outcomes in endodontic microsurgery: a systematic review and meta-analysis. Giornale Italiano di Endondonzia 31( l ) :2-l 3
De Chevigny C, Dao TT, Basrani BR, Marquis V, Forzaneh M, Abitbo l S, Friedman S (2008). Treatment outcome in endodontics: the Toronto study – phase 4 initial treatment. J Endod 34( 3); 25 8-26 3
Wang N, Knight K, Dao T, Friedman S (2004). Treatment outcome in endodontics: the Toronto Study. Phases I and II: apical surgery.) Endod 30 (11) :7 5 1 – 76 1
Tsesis I, Rosen E, Taschieri 5 , Telishevsky Strauss Y, Ceresoli V, Del Fabbro M ( 20 1 3) . Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endo d 39( 3): 332 -339
Setzer FC, Koh li M R, Shah SB, Korabucak B, Kim S ( 20 1 2) . Outcome of endodontic surgery: a meta-analysis of the literature – Port 2: Comparison of endodontic rnicrosurgical techniques with and without the use of higher magnification. J Endod 38( l ): l -l 0
Floratos S, Syngcuk K (20 1 7). Modern Endodontic Microsurgery Concepts: A Clinical Update. Dent Cf in N Arn 61 ( lI81-9l
Ahlowalio MS, Patel S, Anwar HM, Corna G, Austin RS, W ilson R, Mannocci F (20 l 3) . Accuracy of CBCT for volumetric measurement of simulated periapical lesions. Int Endod J 46(6):5 38-546
Venskutonis T, Plo tino G, Juodzbalys G, Mickevii’iene L (2014). The importance of cone-beam computed tomography in the management of endodontic problems: a review of the literature. J Endod 40 ( 1 2): 1895 – 1901
Kuhl S, Payer M, Zitzman n NU, Lambrecht JT, Filippi A (20 1 5). Technical accuracy of printed surgical templates for guided implant surgery with the co DiagnostiX software Clin Implant Dent Re/at Res l7 Supplier l77 -82
D’Hoese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H (20 l 2). Accurac y and complications using computer designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the lite1·ature. Clin Implant Dent Re/at Res 14(3) 32 1 -335
Pinsky HM, Champ leboux G, Sarment DP (2007). PeriapicaI surgery using CAD/CAM guidance: preclinical results. J Endad 33(2) 14 8-15 1
Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C (2017) Guided Modern Endodontic Surgery: A Novel Approach for Guided Osteotomy and Root Resection. J Endod 43(3):496-50 l
Abella F, d e Ribot J, Doria G, Dura n-Sindreu F, Roig M (20 1 4). Applications of piezoelectric surgery in endodontic surgery: a literature review J Endod 40 ( 3): 325 -5 32
Stropko JJ ( 1999), Canal morphology of maxillary molars: clinical
observations of canal configurations. J Endod 25(6) :446-450
Hw ang JI, Chuang AH, Sidow SJ, M cN ally K, GoodinJL, McPherson JC 3rd (20 1 5). The effectiveness of endodontic solvents to remove endodontic sealers. Mil Med 180 (3 Supp l) 9 2-95
Reprinted with permission from ENDODONTIC PRACTICE February 2019